Imagining the Future of "Code Blue"
Cardiac arrest management today is a mess. What might a future automated approach look like?
Motivation
Once a week or so, I run a Code Blue - hospital speak for a cardiac arrest.
When a patient stops breathing and loses their pulse every second becomes of the essence. Time is brain, time is heart, time is life. A moments delay in starting resuscitation or small imperfections in our technique can drastically affect whether a patient lives or dies.
I’ve worked in hospitals that run like well-oiled machines, and others that squeak and creak at every turn. But even in the best of cases, cardiac arrests are a mess.
Why?
Urgency often turns into panic, and panic into disarray. In fact, even when a team keeps its cool, the complexity of resuscitation and the number of variables at play make it difficult to consistently get everything right.
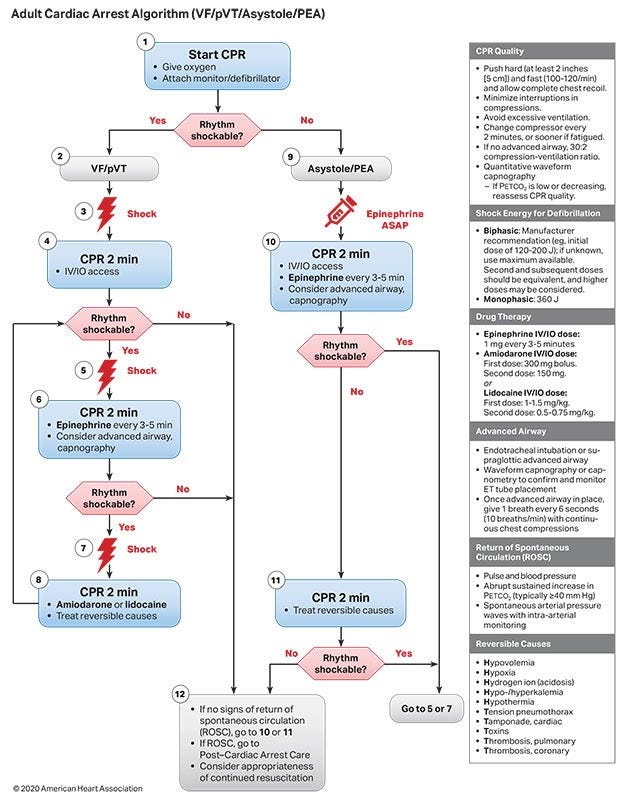
Below is the textbook standard, vastly simplified algorithm for running cardiac arrests.
Each and every one of these steps is a potential failure point. Compressions too slow, too fast, too shallow, or too deep, rhythm strips misinterpreted, wrong shock voltage, bad pad placement, wrong medications, wrong doses, poor ventilation, and the list goes on and on and on.
For these reasons, cardiac arrests are yet another domain in which significant automation will undoubtedly someday become the norm.
As a general rule, any time a complex algorithm such as this one rears its ugly head, think: automation.
So below is a sketch of an imagined, automated system for managing Code Blue’s. Apologies if it gets occasionally technical. The driving principles are:
Plug-and-play: quick and easy initiation, followed by autopilot management
Data driven: resuscitation efforts are informed by real-time biodata not discretion
Maximum Automation: minimize involve human intervention to minimize delay and error
Most of the technology exists or can be built with off-the shelf components.
Automated Cardiac Arrest Management
The components of the system are:
Central Command AI
Code Blue Team Members
Infrastructure and Equipment
Central Command AI
The brains of the operation. Acts on critical inputs and outputs:
A. Inputs:
Biosensor data (3/12 lead ECG, EtCO2, Peak Pressures, etc.)
EMR data (clinical context, medical history, radiography, etc.)
Real-time team member data (task status, manually reported complications, etc.)
Cutting edge clinical practice guidelines and trained nets
B. Outputs:
CPR mechanics management (Ventilation, LUCAS-like device management)
Medication/blood product administration
Team task delegation
Radiography management and interpretation
Automated EMR logging
Thermoregulation
Specialist service activation and coordination
Code Blue Team Members
In the short term, we’re unlikely to have complete automation. Critical team member roles include:
Airway: VL intubation, connection to the ventilatory apparatus which is integrated
Access: PIV, IO, CVC, and connect to integrated tubing and Medication Management Module
Procedural: Needle decompression, thoracotomy, pericardiocentesis, REBOA
Imaging: Sonography, other non-automated imaging (Plain films via a detector integrated in the stretcher and an overhead XR tube for automated imaging and interpretation)
Communication between Central Command and team members is one-to-one via an earpiece or mobile device. Each item completed is checked off which provides closed loop feedback to Central Command.
Importantly, once airway and other elements are established by team members they are not responsible for ongoing management. That role reverts back to the automated Central Command. The idea is to build a plug and play model wherein the patient is plugged into a resuscitation infrastructure that automatically manages the code.
Infrastructure and Equipment
We need new equipment to make this work which includes:
A Code Blue Bed with various integrated peripherals:
Wireless biosensors (Wireless ECG sensors, EtCO2, pulse oximetry, etc.)
Integrated Medication Management Module (tubing to MedStation. automated dispensation of ACLS medications, connects directly to IO, PIV, CVC, etc.)
Integrated Ventilation Management Module (connects directly to ETT or supraglottic airway, sensors feed into Automated Central Command)
Integrated Thermostasis Module (cooling (for hypothermia protocol, warming for hypothermic patients, etc.)
Integrated Imaging Modules (X-ray Detector, Sonography Probe,
Integrated Circulation Management Module (External compression via LUCAS-like Device, Internal Circulation via rapidly implantable intravascular pump)
Mobile devices, earpieces, AR glasses for Central Command-team member communication
Overhead X-tube/C-Arm Tomography for real-time imaging
Rapidly implantable biosensors (A-line like, real-time biomarker monitoring)
Workflow
A cardiac arrest patient is coming in by EMS or the a patient in the hospital goes into cardiac arrest. The workflow proceeds as follows:
High quality CPR initiated immediately
Big Blue Button pushed - Code Blue Activated
Team members with preordained, highly trained roles dispatched
Central Command AI assumes control
ASAP transfer the patient to a “Code Blue Bed” and into the “Code Blue Bay” (alternatively every hospital bed in the future is a “Resuscitation Bed”)
Patient plugged into peripherals by team members (airway, vascular access, compression device, etc.)
Patient automatically recognized by facial recognition or other identifying information and clinical context invoked
From here on Code Blue is automated and dictated by Central Command AI
Two possible endpoints:
Cessation of resuscitative efforts: this is a function of statistical analysis not clinician discretion
Return of Spontaneous Circulation - initiation of post-arrest care
At first the Automated Central Command makes decisions based on known best practices. Later on, it will come to define best practices by recognizing what works and what doesn’t. Decisions once made by someone like me are now offloaded to the machine. Central Command adjusts hundreds of effectors in a sub-second timeframe based on incoming data from hundreds of biosensors. This includes:
Closed-loop control of CPR mechanics (ventilation rate/volume, non-invasive circulation via compression rate/depth, etc.)
Real-time monitoring of functional metrics (Real-time blood gas metrics, including future prognostic indicators)
Automated administration of medications, fluids, blood products, etc. integrated tubing
Team task delegation (e.g. for advanced access for HD or other interventions)
Blood draws or in-vivo laboratory testing
Automated radiography capture, interpretation, and intervention (e.g. overhead X-ray tube, stretcher with embedded detector, automated detection of tension pneumothorax and instruction to proceduralist to perform needle decompression).
Again I’m keen to know what others would add or change so do reach out.
Summary
Cardiac arrests are complex, time sensitive, and high stakes medical moments. Algorithms for managing arrests are well-established but are seldom followed perfectly. It is an area ripe for more automation. Here we’ve imagined a future system that follows a plug-and-play approach. The arresting patient is plugged into a hardware and software infrastructure that is then managed automatically. Biodata is looped back to Central Command which informs resuscitative efforts. Efforts persist until ROSC is established or certain statistical thresholds are reached to cease efforts. Notably it is not left to doctor’s discretion. Like all encounters in a Supermedicine model, each case is a treasure trove of data. The system can thereby iteratively improve care for future cases.